Abstract
Purpose of Review
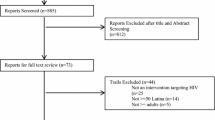
The purpose of this review is to summarize the available evidence-based HIV prevention interventions tailored for transgender people.
Recent Findings
A limited number of evidence-based HIV prevention interventions have been tested with transgender populations. Most existing interventions target behavior change among transgender women, with only one HIV prevention program evaluated for transgender men. Studies addressing biomedical interventions for transgender women are ongoing. Few interventions address social and structural barriers to HIV prevention, such as stigma, discrimination, and poverty.
Summary
Evidence-based multi-level interventions that address the structural, biomedical, and behavioral risks for HIV among transgender populations, including transgender men, are needed to address disparities in HIV prevalence. Future research should address not only pre-exposure prophylaxis uptake and condom use but also structural barriers that limit access to these prevention strategies.
Similar content being viewed by others
Change history
13 September 2017
An erratum to this article has been published.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Center of Excellence for Transgender Health. Guidelines for the primary and gender-affirming care of transgender and gender nonbinary people [updated June 17, 2016; cited 2017 March 26]. Second:[Available from: http://transhealth.ucsf.edu/trans?page=guidelines-home.
•• United Nations Development Programme, IRGT A Global Network of Transgender Women and HIV, United Nations Population Fund, UCSF Center of Excellence for Transgender Health, Johns Hopkins Bloomberg School of Public Health, World Health Organization, et al. Implementing comprehensive HIV and STI programmes with transgender people: practical guidance for collaborative interventions. New York: United Nations Development Programme; 2016. The first global transgender community-led implementation guide for HIV/STI prevention with transgender people
Winter S, Diamond M, Green J, Karasic D, Reed T, Whittle S, et al. Transgender people: health at the margins of society. Lancet. 2016;388(10042):390–400.
Flores AR, Herman JL, Gates GJ, Brown TNT. How many adults identify as transgender in the United States? Los Angeles the Williams Institute 2016. Available from: http://williamsinstitute.law.ucla.edu/wp-content/uploads/How-Many-Adults-Identify-as-Transgender-in-the-United-States.pdf. Accessed 30 June 2017.
Reisner SL, Poteat T, Keatley J, Cabral M, Mothopeng T, Dunham E, et al. Global health burden and needs of transgender populations: a review. Lancet. 2016;388(10042):412–36.
Reisner S, Keatley J, Baral S, Villayzan J, Mothopeng T, van der Merwe LL, et al. Transgender community voices: a participatory population perspective. Lancet. 2016;388(10042):327–30.
Reisner SL, Radix A, Deutsch MB. Integrated and gender-affirming transgender clinical care and research. J Acquir Immune Defic Syndr. 2016;72(Suppl 3):S235–42.
Poteat T, Scheim A, Xavier J, Reisner S, Baral S. Global epidemiology of HIV infection and related syndemics affecting transgender people. J Acquir Immune Defic Syndr. 2016;72(Suppl 3):S210–9.
Baral SD, Poteat T, Strömdahl S, Wirtz AL, Guadamuz TE, Beyrer C. Worldwide burden of HIV in transgender women: a systematic review and meta-analysis. Lancet Infect Dis. 2013;13(3):214–22.
Operario D, Soma T, Underhill K. Sex work and HIV status among transgender women: systematic review and meta-analysis. J Acquir Immune Defic Syndr. 2008;48(1):97–103.
HIV/AIDS. IRGoTPa. Counting trans people. In: Advancing global data collection on transgender communities and HIV Oakland 2016. Available from: http://transglobalactivism.org/counting-trans-people-in-advancing-global-datacollection-on-transgender-communities-and-hiv/.
Habarta N, Wang G, Mulatu MS, Larish N. HIV testing by transgender status at Centers for Disease Control and Prevention—funded sites in the United States, Puerto Rico, and US Virgin Islands. Am J Public Health. 2009–2011;2015:e1–9.
Salazar LF, Crosby RA, Jones J, Kota K, Hill B, Masyn KE. Contextual, experiential, and behavioral risk factors associated with HIV status: a descriptive analysis of transgender women residing in Atlanta, Georgia. Int J STD AIDS. 2017;0(0):1–8.
Silva-Santisteban A, Raymond HF, Salazar X, Villayzan J, Leon S, McFarland W, et al. Understanding the HIV/AIDS epidemic in transgender women of lima, Peru: results from a sero-epidemiologic study using respondent driven sampling (unpublished estimates of transgender sex workers). AIDS Behav. 2012;16(4):872–81.
Guadamuz T, Wimonsate W, Varangrat A, Phanuphak P, Jommaroeng R, McNicholl J, et al. HIV prevalence, risk behavior, hormone use and surgical history among transgender persons in Thailand. AIDS Behav. 2011;15(3):650–8.
Gamarel KE, Reisner SL, Darbes LA, Hoff CC, Chakravarty D, Nemoto T, et al. Dyadic dynamics of HIV risk among transgender women and their primary male sexual partners: the role of sexual agreement types and motivations. AIDS Care. 2016;28(1):104–11.
Operario D, Nemoto T, Iwamoto M, Moore T. Unprotected sexual behavior and HIV risk in the context of primary partnerships for transgender women. AIDS Behav. 2011;15(3):674–82.
Reisner SL, Murchison GR. A global research synthesis of HIV and STI biobehavioural risks in female-to-male transgender adults. Global Public Health. 2016;11(7–8):866–87.
McFarland W, Wilson EC, Raymond HF. HIV prevalence, sexual partners, sexual behavior and HIV acquisition risk among trans men, San Francisco, 2014. AIDS Behav. 2017.
Scheim AI, Bauer GR, Travers R. HIV-related sexual risk among transgender men who are gay, bisexual, or have sex with men. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2017;74(4):e89–96.
McFarland W, Wilson E, Fisher Raymond H. How many transgender men are there in San Francisco? J Urban Health. 2017. doi:10.1007/s10461-017-1735-4.
Bauer GR, Travers R, Scanlon K, Coleman TA. High heterogeneity of HIV-related sexual risk among transgender people in Ontario, Canada: a province-wide respondent-driven sampling survey. BMC Public Health. 2012;12(1):292.
Sturdee DW, Panay N. Recommendations for the management of postmenopausal vaginal atrophy. Climacteric. 2010;13(6):509–22.
Alvarez H, Marino A, Garcia-Rodriguez JF, Vilas-Sueiro A, Valcarce N, Llibre JM. Immune reconstitution inflammatory syndrome in an HIV-infected patient using subcutaneous silicone fillers. Aids. 2016;30(16):2561–3.
Hariri LP, Gaissert HA, Brown R, Ciaranello A, Greene RE, Selig MK, et al. Progressive granulomatous pneumonitis in response to cosmetic subcutaneous silicone injections in a patient with HIV-1 infection: case report and review of the literature. Archives of pathology & laboratory medicine. 2012;136(2):204–7.
Leonardi NR, Compoginis JM, Luce EA. Illicit cosmetic silicone injection: A recent reiteration of history. Annals of plastic surgery. 2016;77(4):485–90.
Murariu D, Holland MC, Gampper TJ, Campbell CA. Illegal silicone injections create unique reconstructive challenges in transgender patients. Plast Reconstr Surg. 2015;135(5):932e–3e.
Wilson E, Rapues J, Jin H, Raymond HF. The use and correlates of illicit silicone or “fillers” in a population-based sample of transwomen, San Francisco, 2013. J Sex Med. 2014;11(7):1717–24.
Benotsch EG, Zimmerman RS, Cathers L, Pierce J, McNulty S, Heck T, et al. Non-medical use of prescription drugs and HIV risk behaviour in transgender women in the mid-Atlantic region of the United States. Int J STD AIDS. 2016;27(9):776–82.
Keuroghlian AS, Reisner SL, White JM, Weiss RD. Substance use and treatment of substance use disorders in a community sample of transgender adults. Drug Alcohol Depend. 2015;152:139–46.
Travers R, Bauer GR, Coleman TA, Scanlon K. Hormone, silicone, and drug injection: assessment of HIV-related injection risk among transgender people in Ontario, Canada [abstract P238]. Can J Infect Dis Med Microbiol. 2012;23(Supplement SA):109A.
Singer M, Clair S. Syndemics and public health: reconceptualizing disease in bio-social context. Med Anthropol Q. 2003;17(4):423–41.
Tsai AC, Venkataramani AS. Syndemics and health disparities: a methodological note. AIDS Behav. 2016;20(2):423–30.
Baral S, Logie CH, Grosso A, Wirtz AL, Beyrer C. Modified social ecological model: a tool to guide the assessment of the risks and risk contexts of HIV epidemics. BMC Public Health. 2013;13:482.
• Poteat T, Wirtz AL, Radix A, Borquez A, Silva-Santisteban A, Deutsch MB, et al. HIV risk and preventive interventions in transgender women sex workers. Lancet. 2015;385(9964):274–86. Models impact of HIV prevention interventions specifically for transgender women sex workers
Sevelius JM. Gender affirmation: a framework for conceptualizing risk behavior among transgender women of color. Sex Roles. 2013;68(11–12):675–89.
Reisner SL, White Hughto JM, Pardee D, Sevelius J. Syndemics and gender affirmation: HIV sexual risk in female-to-male trans masculine adults reporting sexual contact with cisgender males. Int J STD AIDS. 2016;27(11):955–66.
•• Garofalo R, Kuhns LM, Reisner SL, Mimiaga MJ. Behavioral interventions to prevent HIV transmission and acquisition for transgender women: a critical review. J Acquir Immune Defic Syndr. 2016;72(Suppl 3):S220–5. Review and critique of behavioral HIV preventoin interventions for transgender women
Garofalo R, Johnson AK, Kuhns LM, Cotten C, Joseph H, Margolis A. Life skills: evaluation of a theory-driven behavioral HIV prevention intervention for young transgender women. J Urban health Bull NYAcad Med. 2012;89(3):419–31.
Gutierrez-Mock L, Thomas-Guess Y, Keatley J, Cotten P, Kegeles S. T-SISTA: a resource guide for adapting SISTA for transwomen of color. San Fransisco: Univ California San Fransisco: The Transitions Project, 2009.
Beyrer C, Baral SD, van Griensven F, Goodreau SM, Chariyalertsak S, Wirtz AL, et al. Global epidemiology of HIV infection in men who have sex with men. Lancet. 2012;380(9839):367–77.
Poteat T, Reisner SL, Radix A. HIV epidemics among transgender women. Curr Opin HIV AIDS. 2014;9(2):168–73.
Nemoto T, Operario D, Keatley J, Nguyen H, Sugano E. Promoting health for transgender women: Transgender Resources and Neighborhood Space (TRANS) program in San Francisco. Am J Public Health. 2005;95(3):382–4.
Taylor RD, Bimbi DS, Joseph HA, Margolis AD, Parsons JT. Girlfriends: evaluation of an HIV-risk reduction intervention for adult transgender women. AIDS Educ Prev Off Publ Int Soc AIDS Educ. 2011;23(5):469–78.
Pawa D, Firestone R, Ratchasi S, Dowling O, Jittakoat Y, Duke A, et al. Reducing HIV risk among transgender women in Thailand: a quasi-experimental evaluation of the sisters program. PLoS One. 2013;8(10):e77113.
Longfield K, Panyanouvong X, Chen J, Kays MB. Increasing safer sexual behavior among Lao kathoy through an integrated social marketing approach. BMC Public Health. 2011;11:872.
•• World Health Organization. WHO guidelines approved by the guidelines review committee. Consolidated guidelines on HIV prevention, diagnosis, treatment and care for key populations—2016 update. Geneva: World Health Organization; 2016. Current global guidelines for key populations along the HIV prevention and care continuum
Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–99.
•• Deutsch MB, Glidden DV, Sevelius J, Keatley J, McMahan V, Guanira J, et al. HIV pre-exposure prophylaxis in transgender women: a subgroup analysis of the iPrEx trial. Lancet HIV. 2015;2(12):e512–9. The only transgender-specific analysis of PrEP efficacy
Department of Health and Human Services. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents [updated July 14, 2016; cited 2017 June 26]. Available from: https://aidsinfo.nih.gov/guidelines/html/1/adult-and-adolescent-arv-guidelines/286/nrti-drug-interactions.
Louissaint NA, Cao YJ, Skipper PL, Liberman RG, Tannenbaum SR, Nimmagadda S, et al. Single dose pharmacokinetics of oral tenofovir in plasma, peripheral blood mononuclear cells, colonic tissue, and vaginal tissue. AIDS Res Hum Retrovir. 2013;29(11):1443–50.
Shen Z, Fahey JV, Bodwell JE, Rodriguez-Garcia M, Kashuba AD, Wira CR. Sex hormones regulate tenofovir-diphosphate in female reproductive tract cells in culture. PLoS One. 2014;9(6):e100863.
Lade JM, To EE, Hendrix CW, Bumpus NN. Discovery of genetic variants of the kinases that activate tenofovir in a compartment-specific manner. EBioMedicine. 2015.
AVAC: Global Advocacy for HIV Prevention. Ongoing and planned PrEP open label, demonstration and implementation projects 2017 [updated May 30, 2017; cited 2017 June 20]. Available from: http://www.avac.org/resource/ongoing-and-planned-prep-demonstration-and-implementation-studies.
California HIV/AIDS Research Program. Prevention and linkage to care: active grants [cited 2017 June 19]. Available from: http://www.californiaaidsresearch.org/funded-research/current%20prevention%20and%20linkage%20to%20care%20awards.html.
NIH Research Portfolio Online Reporting Tools [cited 2017 June 1]. Available from: https://projectreporter.nih.gov/reporter.cfm.
Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Antiretroviral therapy for the prevention of HIV-1 transmission. N Engl J Med. 2016;375(9):830–9.
Rodger AJ, Cambiano V, Bruun T, et al. Sexual activity without condoms and risk of hiv transmission in serodifferent couples when the hiv-positive partner is using suppressive antiretroviral therapy. JAMA. 2016;316(2):171–81.
Health Resources and Services Administration Ryan White & Global HIV/AIDS Programs. Enhancing engagement and retention in quality HIV care for transgender women of color [cited 2017 June 20]. Available from: https://hab.hrsa.gov/about-ryan-white-hivaids-program/spns-transgender-women-color.
• Rebchook G, Keatley J, Contreras R, Perloff J, Molano LF, Reback CJ, et al. The transgender women of color initiative: implementing and evaluating innovative interventions to enhance engagement and retention in HIV care. Am J Public Health. 2017;107(2):224–9. Describes the first paper focused improving engagement in HIV care for transgender women of color living with HIV
Adimora AA, Auerbach JD. Structural interventions for HIV prevention in the United States. J Acquir Immune Defic Syndr. 2010;55(Suppl 2):S132–5.
Frieden TR. A framework for public health action: the health impact pyramid. Am J Public Health. 2010;100(4):590–5.
Reisner SL, Perez-Brumer AG, SA ML, Lama JR, Silva-Santisteban A, Huerta L, et al. Perceived barriers and facilitators to integrating HIV prevention and treatment with cross-sex hormone therapy for transgender women in Lima. Peru.: AIDS Behav; 2017.
Perez-Brumer AG, Reisner SL, McLean SA, Silva-Santisteban A, Huerta L, Mayer KH, et al. Leveraging social capital: multilevel stigma, associated HIV vulnerabilities, and social resilience strategies among transgender women in Lima Peru. J Int AIDS Soc. 2017;20(1):1–8.
White Hughto JM, Reisner SL, Pachankis JE. Transgender stigma and health: a critical review of stigma determinants, mechanisms, and interventions. Soc Sci Med (1982). 2015;147:222–31.
Bockting WO, Rosser BR, Scheltema K. Transgender HIV prevention: implementation and evaluation of a workshop. Health Educ Res. 1999;14(2):177–83.
De Santis JP, Martin CW, Lester A. An educational program on HIV prevention for male-to-female transgender women in south Miami Beach, Florida. J Assoc Nurses AIDS Care. 2010;21(3):265–71.
Reisner SL, Hughto JM, Pardee DJ, Kuhns L, Garofalo R, Mimiaga MJ. LifeSkills for men (LS4M): pilot evaluation of a gender-affirmative HIV and STI prevention intervention for young adult transgender men who have sex with men. J Urban Health. 2016;93(1):189–205.
Bockting WO, Robinson BE, Forberg J, Scheltema K. Evaluation of a sexual health approach to reducing HIV/STD risk in the transgender community. AIDS Care. 2005;17(3):289–303.
Collier KL, Colarossi LG, Hazel DS, Watson K, Wyatt GE. Healing our women for transgender women: adaptation, acceptability, and pilot testing. AIDS Educ Prev Off Publ Int Soc AIDS Educ. 2015;27(5):418–31.
Hill BJ, Crosby R, Bouris A, Brown R, Bak T, Rosentel K, et al. Exploring transgender legal name change as a potential structural intervention for mitigating social determinants of health among transgender women of color. Sex Res Soc Pol. 2017:1–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Ayana Elliot has served on the speakers’ bureau for Gilead Sciences Inc.
Tonia Poteat, Mannat Malik, and Ayden Scheim declare that they have no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on The Science of Prevention
An erratum to this article is available at https://doi.org/10.1007/s11904-017-0365-9.
Rights and permissions
About this article
Cite this article
Poteat, T., Malik, M., Scheim, A. et al. HIV Prevention Among Transgender Populations: Knowledge Gaps and Evidence for Action. Curr HIV/AIDS Rep 14, 141–152 (2017). https://doi.org/10.1007/s11904-017-0360-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11904-017-0360-1


