Abstract
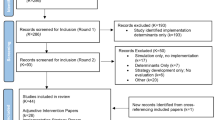
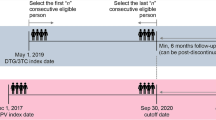
Background There are 34 million people living with human immunodeficiency virus (HIV) worldwide and each year this number increases. Until a vaccine is discovered, the prevention of new HIV infections remains an urgent priority. Several trials studying the use of oral and topical agents for the prevention of HIV infection have already been completed. Adherence has proved to be a major challenge in achieving product efficacy. Aim of the review To provide the clinical pharmacist with an understanding of the oral pre-exposure prophylaxis (PrEP) and topical microbicide product pipeline whilst emphasizing the critical importance of adherence to these drugs to avert HIV infection. Methods PubMed/Medline and the web-based clinical trials registry (ClinTrials.gov) were searched using appropriate key words. For the time period 1992–2013—all phase II and phase III safety and effectiveness studies—testing agents for prevention of HIV infection were included in the review. Efficacy estimates, adherence estimates and reported challenges with adherence were extracted. Results Twenty-four phase II and III clinical trials were found during review. Of these, 20 trials have been completed, and six trials show effectiveness in preventing HIV infection. The majority of the successful trials were to oral PrEP and to date only one microbicide trial of a vaginal antiretroviral microbicide gel has showed effectiveness. Adherence to study product played a major role in trial outcomes and there are several reasons for non-adherence. These include high on-trial pregnancy rates, low trial retention rates, low participant perception of risk, participant characteristics such as age <25 years, single status, migratory partners and trial fatigue. Study product characteristics such as dosage form, dosing interval, as well as associated adverse events may also influence adherence. Conclusion Moderate to high adherence is critical to demonstrate efficacy of drugs for HIV prevention. For topical agents, intermittent use associated with coitus is more effective than daily use, particularly if sex is infrequent or partners migrant. For oral agents, daily use is effective but the motivation to use the drug and high risk perception is important. In serodiscordant couples, early initiation of highly active antiretroviral therapy in the infected partner affords almost complete protection to the negative partner. Drugs need to be tailored to the population at risk and availability of multiple drug options are important.

Similar content being viewed by others
References
UNAIDS. Global report: UNAIDS report on the global AIDS epidemic 2012. Available from: Geneva: joint united nations programme on HIV/AIDS. Accessed 25 Mar 2013.
Leclerc-Madlala S. Age-disparate and intergenerational sex in southern Africa: the dynamics of hypervulnerability. AIDS. 2008;22(Suppl 4):S17–25.
Stone A, Harrison PF. Microbicides—ways forward. Silver Spring: Alliance for Microbicide Development; 2010.
Veronese F, Anton P, Fletcher CV, DeGruttola V, McGowan I, Becker S, et al. Implications of HIV PrEP trials results. AIDS Res Hum Retrovirus. 2011;27(1):81–90.
US Food and Drug Administration. FDA approves first drug for reducing the risk of sexually acquired HIV infection. Available from Silver Spring, MD 2012. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm312210.htm. Accessed 19 July 2012.
Ware NC, Wyatt MA, Haberer JE, Baeten JM, Kintu A, Psaros C, et al. What’s love got to do with it? Explaining adherence to oral antiretroviral pre-exposure prophylaxis for HIV-serodiscordant couples. J AIDS. 2012;59(5):463–8.
Amico KR, Mansoor LE, Corneli A, Torjesen K, van der Straten A. Adherence support approaches in biomedical HIV prevention trials: experiences, insights and future directions from four multisite prevention trials. AIDS Behav. 2013;17(6):2143–55.
Woodsong C, Macqueen K, Amico KR, Friedland B, Gafos M, Mansoor L, et al. Microbicide clinical trial adherence: insights for introduction. J Int Aids Soc. 2013;16:18505.
Ferrer RA, Morrow KM, Fisher WA, Fisher JD. Toward an information-motivation-behavioral skills model of microbicide adherence in clinical trials. AIDS Care. 2010;22(8):997–1005.
Roberts ET, Matthews DD. HIV and chemoprophylaxis, the importance of considering social structures alongside biomedical and behavioral intervention. Soc Sci Med. 2012;75(9):1555–61.
Muchomba FM, Gearing RE, Simoni JM, El-Bassel N. State of the science of adherence in pre-exposure prophylaxis and microbicide trials. J AIDS. 2012;61(4):490–8.
Baeten JM, Donnell D, Ndase P, Mugo NR, Campbell JD, Wangisi J, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med. 2012;367(5):399–410.
Marrazzo JRG, Nair G, Palanee T, Mkhize B, Nakabiito C, Taljaard M, Piper J, Gomez Feliciano K, Chirenje M. VOICE study team: pre-exposure prophylaxis for HIV in women: daily oral tenofovir, oral tenofovir/emtricitabine, or vaginal tenofovir gel in the voice study (MTN003). Abstract#26LB. Conference of Retroviral and Opportunistic Infections; Georgia World Congress Centre, Atlanta, USA 2013.
MicrobicideTrialsNetwork. MTN 003: Phase 2B safety and effectiveness study of tenofovir 1% Gel, tenofovir disoproxil fumarate tablet and emtricitabine/tenofovir disoproxil fumarate tablet for the prevention of HIV infection in women. Available from: http://www.mtnstopshiv.org/node/70. Cited 23 Apr 2013.
Martin MVS, Suntharasamai P, Sangkum U, Leethochawalit M, Chiamwongpaet S, Kittimunkong S, Mock PA, Paxton L, Choopanya K. The Bangkok Tenofovir study group, editor. Participant adherence in the Bangkok Tenofovir Study, an HIV pre-exposure prophylaxis trial in Bangkok. 6th IAS conference on HIV pathogenesis and treatment: abstract no TUPE350; Rome, Italy; 2011.
Choopanya K, Martin M, Suntharasamai P, Sangkum U, Mock PA, Leethochawalit M, et al. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2013;381(9883):2083–90.
Thigpen MC, Kebaabetswe PM, Paxton LA, Smith DK, Rose CE, Segolodi TM, et al. Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in botswana. N Engl J Med. 2012;367(5):423–34.
Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 Infection with early antiretroviral therapy. N Engl J Med. 2011;365:493–505.
Mutua G, Sanders E, Mugo P, Anzala O, Haberer JE, Bangsberg D, et al. Safety and adherence to intermittent pre-exposure prophylaxis (PrEP) for HIV-1 in african men who have sex with men and female sex workers. PLoS ONE. 2012;7(4). doi 10.1371/journal.pone.0033103.
Van Damme L, Corneli A, Ahmed K, Agot K, Lombaard J, Kapiga S, et al. Preexposure prophylaxis for HIV infection among African women. N Engl J Med. 2012;367(5):411–22.
Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–99.
Peterson L, Nanda K, Opoku BK, Ampofo WK, Owusu-Amoako M, Boakye AY, et al. SAVVY® (C31G) gel for prevention of HIV infection in women: a phase 3, double-blind, randomized, placebo-controlled trial in Ghana. PLoS ONE. 2007;2(12):e1312. doi:10.71/journal.pone.0001312.
Amico KR, Liu A, McMahan V, Anderson PL, Lama JR, Guanira J, et al. (eds) Adherence indicators and pre-exposure prophylaxis (PrEP) drug levels in the iPrEx study. Conference on retroviruses and opportunistic infections, Boston, Massachusetts: 2011.
Haberer JE, Psaros C, Baeten J, Katibira E, Tumwesigye E, Ronald A, et al. (eds) High adherence to oral PrEP is associated with lack of infections in an ancillary study of objective adherence monitoring and counseling among HIV discordant couples in partners PrEP study. Conference of retroviruses and opportunistic infections, Seattle, 2012.
Bekker L, Glidden D, Hosek S, Brown B, Liu A, Amico R, et al. editors. Pre-exposure prophylaxis in young men who have sex with men: needs and challenges [Paper #997]. Conference on retroviruses and opportunistic infections. Georgia World Congress Centre, Atlanta, 2013.
World Health Organisation. Coverage of selected health services for HIV/AIDS prevention and care in less developed countries in 2001. Available from http://whqlibdoc.who.int/publications/9241590319.pdf. Geneva, Switzerland: 2002.
Kreiss J, Ngugi E, Holmes K, Ndinya-Achola J, Waiyaki P, Roberts PL, et al. Efficacy of nonoxynol 9 contraceptive sponge use in preventing heterosexual acquisition of HIV in Nairobi prostitutes. JAMA. 1992;268(4):477–82.
Abdool Karim SS, Richardson BA, Ramjee G, Hoffman IF, Chirenje ZM, Taha T, et al. Safety and effectiveness of BufferGel and 0.5 % PRO2000 gel for the prevention of HIV infection in women. AIDS. 2011; 25(7):957–66.
McCormack S, Ramjee G, Kamali A, Rees H, Crook AM, Gafos M, et al. PRO2000 vaginal gel for prevention of HIV-1 infection (Microbicides Development Programme 301): a phase 3, randomised, double-blind, parallel-group trial. Lancet. 2010;376(9749):1329–37.
Skoler-Karpoff S, Ramjee G, Ahmed K, Altini L, Plagianos MG, Friedland B, et al. Efficacy of carraguard for prevention of HIV infection in women in South Africa: a randomised, double-blind, placebo-controlled trial. Lancet. 2008;372(9654):1977–87.
Van Damme L, Govinden R, Mirembe FM, Guedou F, Solomon S, Becker ML, et al. Lack of effectiveness of cellulose sulfate gel for the prevention of vaginal HIV transmission. New Engl J Med. 2008;359(5):463–72.
Roddy RE, Zekeng L, Ryan KA, Tamoufe U, Weir SS, Wong EL. A controlled trial of nonoxynol 9 film to reduce male-to-female transmission of sexually transmitted diseases. N Engl J Med. 1998;339(8):504–10.
Richardson BA, Lavreys L, Martin HL Jr, Stevens CE, Ngugi E, Mandaliya K, et al. Evaluation of a low-dose nonoxynol-9 gel for the prevention of sexually transmitted diseases: a randomized clinical trial. Sex Transm Dis. 2001;28(7):394–400.
Van Damme L, Ramjee G, Alary M, Vuylsteke B, Chandeying V, Rees H, et al. Effectiveness of COL-1492, a nonoxynol-9 vaginal gel, on HIV-1 transmission in female sex workers: a randomised controlled trial. Lancet. 2002;360(9338):971–7.
Feldblum PJ, Adeiga A, Bakare R, Wevill S, Lendvay A, Obadaki F, et al. SAVVY vaginal gel (C31G) for prevention of HIV infection: a randomized controlled trial in Nigeria. PLoS ONE. 2008;3(1):e1474. doi:10.371/journal.pone.0001474.
Halpern V, Ogunsola F, Obunge O, Wang CH, Onyejepu N, Oduyebo O, et al. Effectiveness of cellulose sulfate vaginal gel for the prevention of HIV infection: results of a phase III trial in Nigeria. PLoS ONE. 2008;3(11):e3784. doi:10.1371/journal.pone.0003784.
Abdool Karim Q, Abdool Karim SS, Frohlich JA, Grobler AC, Baxter C, Mansoor LE, et al. Effectiveness and safety of tenofovir gel, an antiretroviral microbicide, for the prevention of HIV infection in women. Science. 2010; 329(5996):1168–74.
ClinicalTrials.gov. FACTS 001: Safety and effectiveness of tenofovir gel in the prevention of human immunodeficiency virus (HIV-1) infection in young women and the effects of tenofovir gel on the incidence of herpes simplex virus (HSV-2) infection. Available from http://clinicaltrials.gov/ct2/show/NCT01386294?term=facts+001&rank=1. Cited 22 Apr 2013.
ClinicalTrials.gov. CAPRISA 008: implementation effectiveness and safety of tenofovir gel provision through family planning services. Available from http://www.clinicaltrials.gov/ct2/show/NCT01691768?term=CAPRISA+008&rank=1. Cited 23 Apr 2013.
Anton PA, Cranston RD, Kashuba A, Hendrix CW, Bumpus NN, Richardson-Harman N, et al. RMP-02/MTN-006: a phase 1 rectal safety, acceptability, pharmacokinetic, and pharmacodynamic study of tenofovir 1% gel compared with oral tenofovir disoproxil fumarate. AIDS Res Hum Retroviruses. 2012;28(11):1412–21.
MicrobicideTrialsNetwork. MTN-017 Backgrounder: phase II safety and acceptability study of tenofovir gel reformulated for rectal use. 2012; Available from http://www.mtnstopshiv.org/news/studies/mtn017/backgrounder. Cited 22 Apr 2013.
ClinicalTrials.gov. IPM 027: Safety and efficacy trial of a dapivirine vaginal matrix ring in healthy HIV-negative women. Available from http://www.clinicaltrials.gov/ct2/show/NCT01539226?term=IPM+027&rank=2. Cited 24 Apr 2013.
ClinicalTrials.gov. MTN 020: phase 3 safety and effectiveness trial of dapivirine vaginal ring for prevention of hiv-1 in women (ASPIRE). Available from http://www.clinicaltrials.gov/ct2/show/NCT01617096?term=mtn+020&rank=1. Cited 24 Apr 2013.
ARV-based prevention research and development product pipeline (database on the Internet). Available from http://www.avac.org/. Cited 30 Apr 2013.
Williams BG, Abdool Karim SS, Karim QA, Gouws E. Epidemiological impact of tenofovir gel on the HIV epidemic in South Africa. J AIDS. 2011; 58(2):207–10.
Anderson PL, Glidden DV, Liu A, Buchbinder S, Lama JR, Guanira JV, et al. Emtricitabine-tenofovir concentrations and pre-exposure prophylaxis efficacy in men who have sex with men. Sci Transl Med. 2012; 4(151):151ra25. doi: 10.1126/scitranslmed.3004006.
van der Straten A, Van Damme L, Haberer JE, Bangsberg DR. Unraveling the divergent results of pre-exposure prophylaxis trials for HIV prevention. AIDS. 2012;26(7):F13–9.
Kahle E, Donnell D, James H, Thomas K, John-Stewart G, Nakku-Joloba E, et al. PrEP has high efficacy for HIV-1 prevention among higher-risk HIV-1 serodiscordant couples: a subgroup analysis from the Partners PrEP Study. J Int Aids Soc. 2012;15:138–9.
Abdool Karim SS, Kashuba A, Werner L, Abdool Karim Q. Drug concentrations following topical and oral antiretroviral pre-exposure prophylaxis: Implications for HIV prevention in women. Lancet. 2011; 378:279–81.
Liu A, Huang Y, Defechereux P, McMahan V, Eden C, Guanira J, et al. editors. Hair as a biological marker of daily oral pre-exposure prophylaxis (PrEP) adherence and tenofovir/emtricitabine (TFV/FTC) exposure in the global iPrEx Study abstract: MOLBPE037. 6th IAS conference on HIV pathogenesis, treatment and prevention. Rome, Italy; 2011.
Tangmunkongvorakul A, Chariyalertsak S, Amico KR, Saokhieo P, Wannalak V, Sangangamsakun T, et al. Facilitators and barriers to medication adherence in an HIV prevention study among men who have sex with men in the iPrEx study in Chiang Mai, Thailand. AIDS Care. 2012; doi: 10.1080/09540121.2012.748871.
Kamali A, Byomire H, Muwonge C, Bakobaki J, Rutterford C, Okong P, et al. A randomised placebo-controlled safety and acceptability trial of PRO 2000 vaginal microbicide gel in sexually active women in Uganda. Sex Trans Infect. 2010;86(3):222–6.
MicrobicideTrialsNetwork. Press Release: trial finds tenofovir gel safe for daily use and most women adhered to study regimens. 2008; Available from http://www.mtnstopshiv.org/node/359. Cited 23 Apr 2013.
Hillier SL. Safety and acceptability of coitally dependent use of 1% tenofovir over 6 months of use. Abstract No. 655. Microbicides 2008 New Delhi, India; 2008.
Hendrix CW, Chen BA, Guddera V, Hoesley C, Justman J, Nakabiito C, et al. MTN-001: randomized pharmacokinetic cross-over study comparing tenofovir vaginal gel and oral tablets in vaginal tissue and other compartments. PLoS ONE. 2013;8(1):e55013. doi:10.1371/journal.pone.0055013.
Minnis AM, Gandham S, Richardson BA, Guddera V, Chen BA, Salata R, et al. Adherence and acceptability in MTN 001: a randomized cross-over trial of daily oral and topical tenofovir for HIV prevention in women. AIDS Behav. 2013;17(2):737–47.
MicrobicideTrialsNetwork. Press release: daily HIV prevention approaches didn’t work for African women in VOICE study. 2013; Available from http://www.mtnstopshiv.org/node/4877. Cited 22 Apr 2013.
MicrobicideTrialsNetwork. Press release: reduced glycerin formulation of tenofovir vaginal gel safe for rectal use 2012; Available from http://www.mtnstopshiv.org/node/4496. Cited 22 Apr 2013.
Acknowledgments
CAPRISA is supported by the National Institute of Allergy and infectious Disease (NIAID), National Institutes of Health (NIH) (Grant No. AI51794). The authors were study personnel in the CAPRISA 004 and CAPRISA 008 Tenofovir gel trials, which was supported by the United States Agency for International Development (USAID), Family Health International (FHI), CONRAD and LIFElab, a biotechnology centre of the South African Department of Science & Technology. The Columbia University-Southern African Fogarty AIDS International Training and Research Programme (AITRP Grant # D43TW00231) has supported Tanuja N Gengiah’s professional development. The views expressed by the authors do not necessarily reflect the views of NIH, USAID, CONRAD, FHI360 or Gilead Sciences.
Funding
None.
Conflicts of interest
The authors have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gengiah, T.N., Moosa, A., Naidoo, A. et al. Adherence challenges with drugs for pre-exposure prophylaxis to prevent HIV infection. Int J Clin Pharm 36, 70–85 (2014). https://doi.org/10.1007/s11096-013-9861-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-013-9861-1