Abstract
Background:
Although early reports have suggested an association between circumcision and prostate cancer (PCa) development, results of subsequent epidemiological studies have been conflicting. Here we examine published articles that explore this association.
Methods:
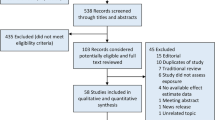
We searched MEDLINE through PubMed and Embase for articles reporting on the association between PCa and circumcision, and performed a meta-analysis of qualifying studies.
Results:
On the basis of seven reports of case–control studies published from 1971 to 2014, overall findings showed nonsignificant reduced risk (odds ratio (OR) 0.88, P=0.19) of PCa in circumcised men compared with uncircumcised men, obtained under heterogeneous conditions (I2=65%). Heterogeneity and nonsignificance were erased when the overall effect was subjected to outlier treatment and three studies omitted (OR 0.90, P=0.04, I2=0%). Furthermore, subgroup analysis showed significantly reduced risks in the following subgroups: (i) post-PSA testing publications (OR 0.88, P=0.01), (ii) population-based studies (OR 0.84, P=0.05), (iii) studies that collected data by personal interview (OR 0.83, P=0.03) and (iv) studies in black race (OR 0.59, P=0.02). The strengths of these summary effects lie in the robustness revealed by sensitivity analysis.
Conclusions:
Stability of the reduced risks observed in key subgroups suggests that the protective feature of circumcision status against PCa is best seen in the context of the post-PSA testing and population-based studies as well as in the black race subgroup.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D . Global cancer statistics. CA Cancer J Clin 2011; 61: 69–90.
Siegel R, Ma J, Zou Z, Jemal A . Cancer statistics, 2014. CA Cancer J Clin 2014; 64: 9–29.
Key T . Risk factors for prostate cancer. Cancer Surv 1995; 23: 63–77.
World Health Organizations, Department of Reproductive Health and Research and Joint United Nations Programme on HIV/AIDS (UNAIDS). Male Circumcision: Global Trends and Determinants of Prevalence, Safety and Acceptability. UNAIDS JUNPoHA, Department of Reproductive Health and Research: Geneva, Switzerland, 2007.
Kaicher DC, Swan KG . A cut above: circumcision as an ancient status symbol. Urology 2010; 76: 18–20.
Morris BJ, Waskett JH, Banerjee J, Wamai RG, Tobian AA, Gray RH et al. A ‘snip’ in time: what is the best age to circumcise? BMC Pediatr 2012; 12: 20.
Rickwood AM . Medical indications for circumcision. BJU Int 1999; 83: 45–51.
Hayashi Y, Kojima Y, Mizuno K, Kohri K . Prepuce: phimosis, paraphimosis, and circumcision. ScientificWorldJournal 2011; 11: 289–301.
Morris BJ . Why circumcision is a biomedical imperative for the 21(st) century. Bioessays 2007; 29: 1147–1158.
Maeda JL, Chari R, Elixhauser A . Circumcisions performed in U.S. community hospitals, 2009: Statistical Brief #126. Healthcare Cost and Utilization Project (HCUP). Agency for Healthcare Research and Quality: Rockville, MD, 2012, pp 1-13. (www.hcup-us.ahrq.gov/reports/statbriefs/sb126.jsp).
Dennis LK, Dawson DV . Meta-analysis of measures of sexual activity and prostate cancer. Epidemiology 2002; 13: 72–79.
Taylor ML, Mainous AG 3rd, Wells BJ . Prostate cancer and sexually transmitted diseases: a meta-analysis. Fam Med 2005; 37: 506–512.
Weiss HA, Quigley MA, Hayes RJ . Male circumcision and risk of HIV infection in sub-Saharan Africa: a systematic review and meta-analysis. AIDS 2000; 14: 2361–2370.
Tobian AA, Serwadda D, Quinn TC, Kigozi G, Gravitt PE, Laeyendecker O et al. Male circumcision for the prevention of HSV-2 and HPV infections and syphilis. N Engl J Med 2009; 360: 1298–1309.
Larke NL, Thomas SL, dos Santos Silva I, Weiss HA . Male circumcision and penile cancer: a systematic review and meta-analysis. Cancer Causes Control 2011; 22: 1097–1110.
Morris BJ, Waskett JH . Circumcision reduces prostate cancer risk. Asian J Androl 2012; 14: 661–662.
Wynder EL, Mabuchi K, Whitmore WF Jr . Epidemiology of cancer of the prostate. Cancer 1971; 28: 344–360.
Mandel JS, Schuman LM . Sexual factors and prostatic cancer: results from a case-control study. J Gerontol 1987; 42: 259–264.
Ross RK, Shimizu H, Paganini-Hill A, Honda G, Henderson BE . Case-control studies of prostate cancer in blacks and whites in southern California. J Natl Cancer Inst 1987; 78: 869–874.
Newell GR, Fueger JJ, Spitz MR, Babaian RJ . A case-control study of prostate cancer. Am J Epidemiol 1989; 130: 395–398.
Ewings P, Bowie C . A case-control study of cancer of the prostate in Somerset and east Devon. Br J Cancer 1996; 74: 661–666.
Rosenblatt KA, Wicklund KG, Stanford JL . Sexual factors and the risk of prostate cancer. Am J Epidemiol 2001; 153: 1152–1158.
Wright JL, Lin DW, Stanford JL . Circumcision and the risk of prostate cancer. Cancer 2012; 118: 4437–4443.
Spence AR, Rousseau MC, Karakiewicz PI, Parent ME . Circumcision and prostate cancer: a population-based case-control study in Montreal, Canada. BJU Int 2014; 114: E90–E98.
Wells GA SB, O'Connell D, Peterson J, Welch V, Losos M, Tugwell P The Newcastle-Ottawa Scale (NOS) for assessing the quality of non-randomised studies in meta-analyses. Ottawa Hospital Research Institute. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed 15 January 2015).
Mantel N, Haenszel W . Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst 1959; 22: 719–748.
DerSimonian R, Laird N . Meta-analysis in clinical trials. Control Clin Trials 1986; 7: 177–188.
Lau J, Ioannidis JP, Schmid CH . Quantitative synthesis in systematic reviews. Ann Intern Med 1997; 127: 820–826.
Berman NG, Parker RA . Meta-analysis: neither quick nor easy. BMC Med Res Methodol 2002; 2: 10.
Higgins JP, Thompson SG . Quantifying heterogeneity in a meta-analysis. Stat Med 2002; 21: 1539–1558.
Galbraith RF . A note on graphical presentation of estimated odds ratios from several clinical trials. Stat Med 1988; 7: 889–894.
Pabalan N, Bapat B, Sung L, Jarjanazi H, Francisco-Pabalan O, Ozcelik H . Cyclin D1 Pro241Pro (CCND1-G870A) polymorphism is associated with increased cancer risk in human populations: a meta-analysis. Cancer Epidemiol Biomarkers Prev 2008; 17: 2773–2781.
Ioannidis JP, Trikalinos TA . The appropriateness of asymmetry tests for publication bias in meta-analyses: a large survey. CMAJ 2007; 176: 1091–1096.
Moher D, Liberati A, Tetzlaff J, Altman DG . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6: e1000097.
Morris BJ, Waskett J, Bailis SA . Case number and the financial impact of circumcision in reducing prostate cancer. BJU Int 2007; 100: 5–6.
Spitz MR, Fueger JJ, Newell GR . The development of a comprehensive, institution-based patient risk evaluation program: II. Validity and reliability of questionnaire data. Am J Prev Med 1988; 4: 188–193.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Pabalan, N., Singian, E., Jarjanazi, H. et al. Association of male circumcision with risk of prostate cancer: a meta-analysis. Prostate Cancer Prostatic Dis 18, 352–357 (2015). https://doi.org/10.1038/pcan.2015.34
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pcan.2015.34